Flexor Tendon Laceration
- Mechanism
- Timing of injury
- Other locations of pain/Associated injuries
- Fractures seen in about 50%
- Numbness/tingling
- Hand dominance
- Profession
Vitals
- Swelling about the metacarpals
- Pain with palpation
- Poke holes or punctate wounds → open injuries
- Dorsal wounds are almost always open fractures
- Do not miss this ; if seen, give IV ancef immediately
- Distal sensation on ulnar and radial side of the injured finger
- Two point discrimination
- Capillary refill
- Will likely be pain limited
- Extension of DIPJ, PIPJ, MCPJ, Wrist
- Extensor tendons can be lacerated
- Flexion of the DIPJ, PIPJ, MCPJ, Wrist
- Ask patient to make a fist - this is important to assess malrotation of the digits
- This is important to assess for malrotation of the digits
- There should be no scissoring (overlap) of the digits
- The fingers should all point to the scaphoid
-

- AP/Lateral/Oblique of involved ray and hand
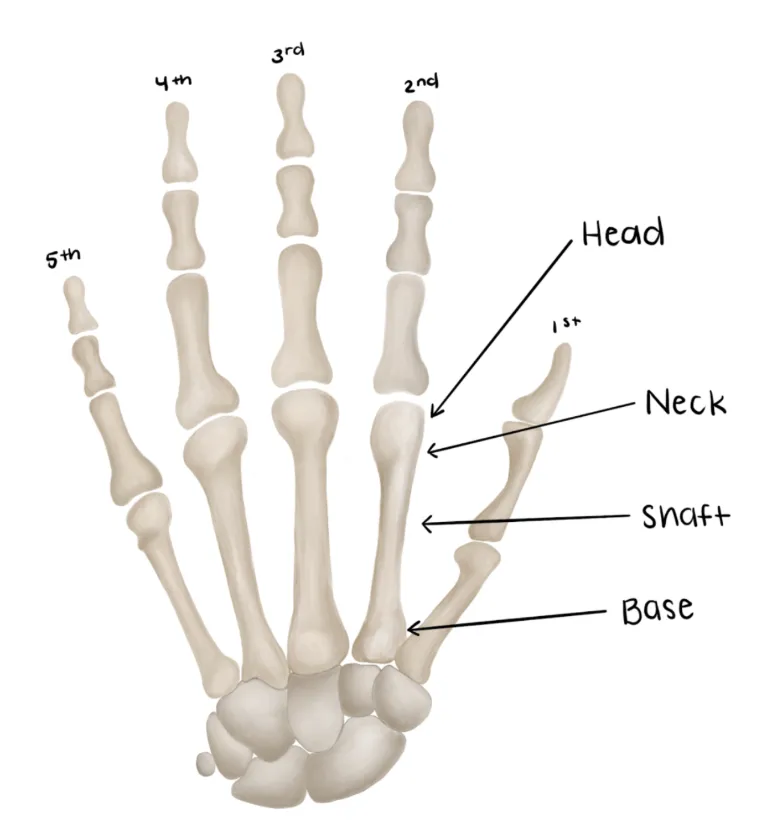
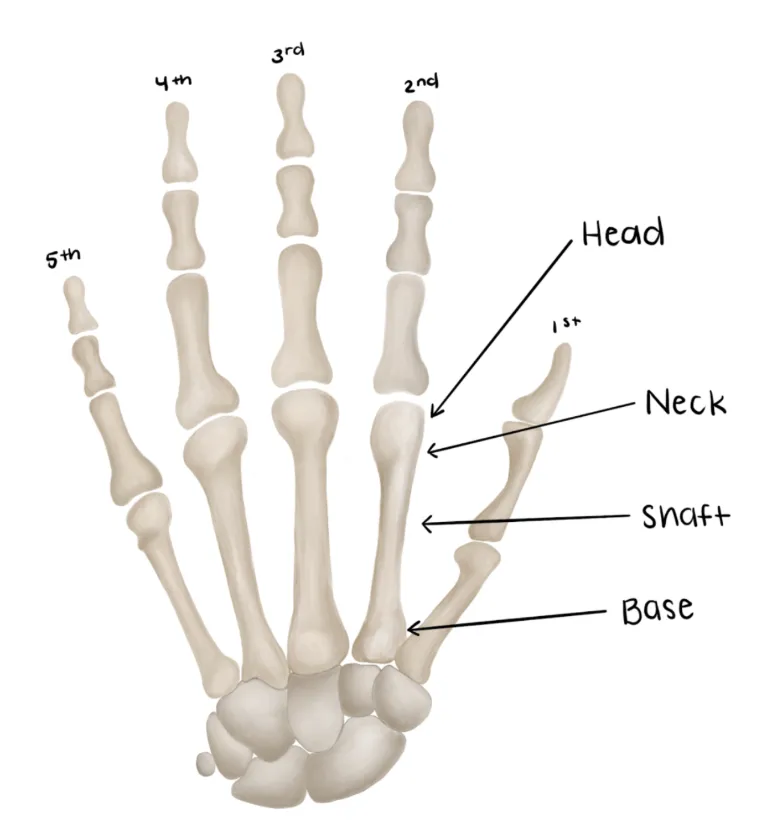
- Describe the location of the fracture based on the bony anatomy below
-
- Acceptable alignment parameters:
| Acceptable Shaft Angulation (degrees) | Acceptable Shaft Shortening (mm) | Acceptable Neck Angulation (degrees) | |
|---|---|---|---|
| Index & Long Finger | 10-20 | 2-5 | 10-15 |
| Ring Finger | 30 | 2-5 | 30-40 |
| Little Finger | 40 | 2-5 | 50-60 |
Medical Decision Making
Closed metacarpal fracture
*** is a *** y/o ***-hand dominant individual with hx of *** who presents with an injury to the *** hand which occurred while mechanism***, found to have an 1st-5th metacarpal*** fracture. On exam, the patient is neurovascularly intact with well perfused digits. The injury was closed with no poke holes or punctate wounds. Radiographs reveal ***. There was/was not*** malrotation of the digit when a fist was made. The fracture was/was not*** reduced under fluoroscopy and immobilized in a radial gutter/ulnar gutter/thumb spica splint***. Post reduction XRs show adequate angulation, and no shortening. The patient will follow up in a hand clinic within one week.
Open metacarpal fracture
*** is a *** y/o ***-hand dominant individual with hx of *** who presents with an injury to the *** hand which occurred while mechanism***, found to have an open 1st-5th metacarpal*** fracture. On exam, the patient is neurovascularly intact with well perfused digits. There was noted to be an open wound which probes to bone. The patient was given an immediate dose of IV ancef/gentamicin***. Orthopaedics was consulted and the patient was made NPO. Radiographs reveal ***. The fracture was immobilized in a radial gutter/ulnar gutter/thumb spica splint***. Orthopaedic surgery to admit the patient and assume care.
If open fracture or traumatic arthrotomy:
- Consult orthopaedic surgery immediately
- NPO, preop labs (type and screen, INR, aPTT, CBC, BMP)
- WB status: Non-weight bearing injured hand
- Diet: Regular
- Analgesia: short course of narcotic pain medication, tylenol (scheduled)
- Ex: 5mg oxycodone q4 - 15 pills
- Immobilization
- Ulnar/Radial Gutter or Thumb Spica +/- reduction (see procedures below)
- 1st metacarpal = thumb spica splint
- 2nd/ metacarpal = radial gutter splint
- 3rd/4th/5th metacarpal = ulnar gutter splint
- Assess angulation/displacement based on the parameters above
- If grossly aligned, hand should be splinted without reduction
- If grossly malaligned, attempt closed reduction & splinting
- As always, if you feel uncomfortable with the reduction, consult orthopaedic surgery
- Disposition: Home with follow up in hand surgery clinic in 1 week
Materials for Splints:

- Trauma Shears,

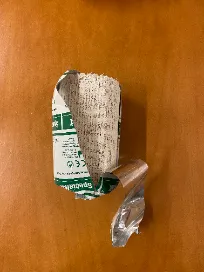
- Webril
 vs. Cast Padding
vs. Cast Padding , depending on institution (multiple),
, depending on institution (multiple), - 4’’ plaster (multiple),
- Bias wrap
 vs.ACE wrap
vs.ACE wrap , depending on institution (multiple),
, depending on institution (multiple), - 1’’ silk tape roll,

- Bucket (filled with warm water),

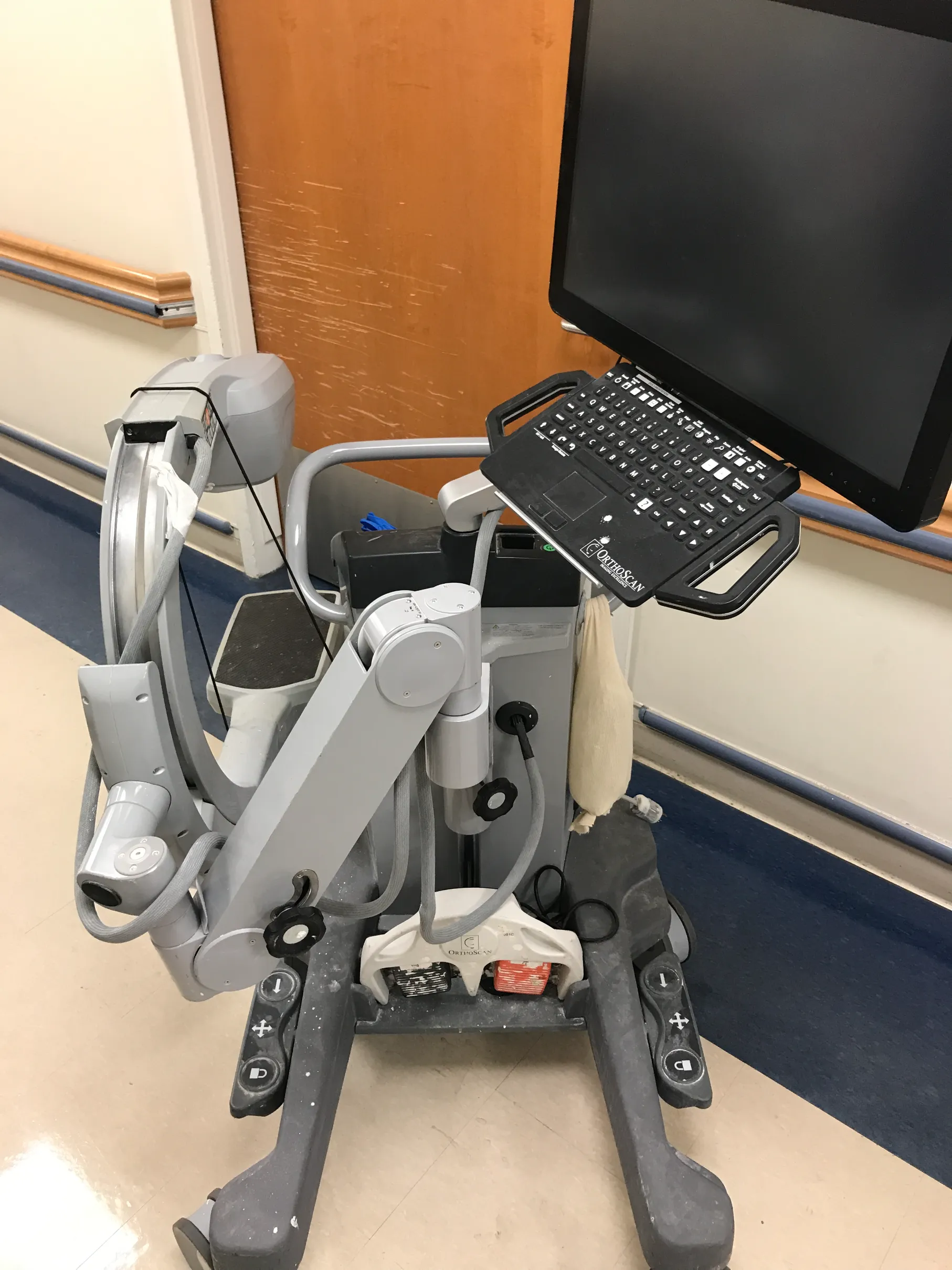
- C-arm fluoroscope ,
- Lead apron (multiple)

Procedure Walkthroughs:
- Position: Wrist in 30 degrees of extension, MCP joints flexed 90 degrees, interphalangeal (IP) joints extended
- Apply soft padding liberally over forearm and ulnar digits (4th/5th digits)
- After wetting, use the plaster/orthoglass to sandwich the ulnar border digits coming from the ulnar side
- Wrist in 30 degrees of extension, MCP joints flexed 90 degrees, interphalangeal (IP) joints extended
- Apply soft padding liberally over forearm and the 2nd/3rd digits
- Radial gutter splint should include a hole cut out for thumb function
- After wetting, use the plaster/orthoglass to sandwich the 2nd/3rd border digits coming from the radial side
- Position: as if holding a can of soda
- Apply soft padding liberally over the thumb, wrist, and distal forearm
- Split/cut the plaster/orthoglass longitudinal with its length on one end
- After wetting, use the split end to cocoon the first ray with the hand in the position as if holding a can of soda
- Pain control with PO or IV analgesics
- Reduction
- Metacarpal Neck Fracture - Jahss Maneuver
-
- Flex the MCPJ to 90 degrees
- Place dorsal pressure through the proximal phalanx when stabilizing the metacarpal shaft
- Metacarpal Shaft Fracture
- A combination of in line traction and pressure over the apex of the deformity can typically reduce these fractures
- Inherently stable and majority are minimally displaced
- Splinting
- 1st Metacarpal fracture
- Use a thumb spica splint for first metacarpal fractures
- See above for details
- 2nd Metacarpal fracture
- Apply a radial gutter splint in intrinsic plus position
- See above for details
- 3rd-5th Metacarpal fracture
- Apply ulnar gutter splint in intrinsic plus position
- See above for details
Procedure Notes:
PROCEDURE NOTE - Application of an Radial Gutter Splint
PRE-PROCEDURE DIAGNOSIS: fracture of the [R/L***] *** metacarpal
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: None
NAME OF PROCEDURE: Application of an Radial Gutter Splint
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain, numbness, and stiffness. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed with the procedure. A timeout was performed.
No attempt at reduction was made. A radial gutter splint was applied. Formal post reduction films showed unchanged alignment. The patient's neurovascular status was consistent with baseline.
COMPLICATIONS: ***
DISPOSITION:
Discharged home with follow up with orthopaedic surgery in 1 week for repeat evaluation
PRE-PROCEDURE DIAGNOSIS: fracture of the [R/L***] *** metacarpal
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: None
NAME OF PROCEDURE: Application of an Radial Gutter Splint
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain, numbness, and stiffness. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed with the procedure. A timeout was performed.
No attempt at reduction was made. A radial gutter splint was applied. Formal post reduction films showed unchanged alignment. The patient's neurovascular status was consistent with baseline.
COMPLICATIONS: ***
DISPOSITION:
Discharged home with follow up with orthopaedic surgery in 1 week for repeat evaluation
PROCEDURE NOTE - Application of an Radial Gutter Splint
PRE-PROCEDURE DIAGNOSIS: fracture of the >[R/L***] *** metacarpal
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: None
NAME OF PROCEDURE: Application of an Radial Gutter Splint
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain, numbness, and stiffness. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed with the procedure. A timeout was performed.
No attempt at reduction was made. A radial gutter splint was applied. Formal post reduction films showed unchanged alignment. The patient's neurovascular status was consistent with baseline.
COMPLICATIONS: ***
DISPOSITION:
Discharged home with follow up with orthopaedic surgery in 1 week for repeat evaluation
PRE-PROCEDURE DIAGNOSIS: fracture of the >[R/L***] *** metacarpal
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: None
NAME OF PROCEDURE: Application of an Radial Gutter Splint
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain, numbness, and stiffness. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed with the procedure. A timeout was performed.
No attempt at reduction was made. A radial gutter splint was applied. Formal post reduction films showed unchanged alignment. The patient's neurovascular status was consistent with baseline.
COMPLICATIONS: ***
DISPOSITION:
Discharged home with follow up with orthopaedic surgery in 1 week for repeat evaluation
PROCEDURE NOTE - Application of an Thumb Spica Splint
PRE-PROCEDURE DIAGNOSIS: Fracture of the [R/L***] 1st metacarpal
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: None
NAME OF PROCEDURE: Splinting of the [R/L***] 1st metacarpal fracture
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain, stiffness, numbness, and tingling. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed with the procedure. A timeout was performed.
No attempts at reduction were made. A well-padded thumb spica splint was applied to the injured hand. Post splint radiographs showed unchanged alignment after the in-situ splinting. The patient's neurovascular status was consistent with baseline.
COMPLICATIONS: ***
DISPOSITION:
Discharged home with follow up with orthopaedic surgery in 1 week for repeat evaluation
PRE-PROCEDURE DIAGNOSIS: Fracture of the [R/L***] 1st metacarpal
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: None
NAME OF PROCEDURE: Splinting of the [R/L***] 1st metacarpal fracture
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain, stiffness, numbness, and tingling. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed with the procedure. A timeout was performed.
No attempts at reduction were made. A well-padded thumb spica splint was applied to the injured hand. Post splint radiographs showed unchanged alignment after the in-situ splinting. The patient's neurovascular status was consistent with baseline.
COMPLICATIONS: ***
DISPOSITION:
Discharged home with follow up with orthopaedic surgery in 1 week for repeat evaluation
PROCEDURE NOTE - Closed Reduction and Splinting of the [R/L***] *** metacarpal/s
PRE-PROCEDURE DIAGNOSIS: fracture of the *** metacarpal/s
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: IV analgesia
NAME OF PROCEDURE: Closed Reduction and Splinting of the *** metacarpal/s
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain and stiffness. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed with the procedure. A timeout was performed.
After IV analgesia was administered to the patient and provided adequate time for analgesic effect, the metacarpal was reduced using a combination of traction and pressure over the apex of the deformity. Gross improvement in alignment was observed and confirmed under fluoroscopic guidance.
A well-padded ulnar/radial gutter/thumb spica splint was then applied to the injured hand with care to maintain the hand in the intrinsic plus position. Fluoroscopic c-arm images showed improved alignment. The patient's neurovascular status was consistent with baseline.
NUMBER OF REDUCTION ATTEMPTS: ***
COMPLICATIONS: ***
DISPOSITION:
Discharged home with follow up with orthopaedic surgery in 1 week for repeat evaluation
PRE-PROCEDURE DIAGNOSIS: fracture of the *** metacarpal/s
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: IV analgesia
NAME OF PROCEDURE: Closed Reduction and Splinting of the *** metacarpal/s
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain and stiffness. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed with the procedure. A timeout was performed.
After IV analgesia was administered to the patient and provided adequate time for analgesic effect, the metacarpal was reduced using a combination of traction and pressure over the apex of the deformity. Gross improvement in alignment was observed and confirmed under fluoroscopic guidance.
A well-padded ulnar/radial gutter/thumb spica splint was then applied to the injured hand with care to maintain the hand in the intrinsic plus position. Fluoroscopic c-arm images showed improved alignment. The patient's neurovascular status was consistent with baseline.
NUMBER OF REDUCTION ATTEMPTS: ***
COMPLICATIONS: ***
DISPOSITION:
Discharged home with follow up with orthopaedic surgery in 1 week for repeat evaluation
PROCEDURE NOTE - Closed Reduction and Splinting of the [R/L***] *** metacarpal/s
PRE-PROCEDURE DIAGNOSIS: fracture of the *** metacarpal/s neck
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: IV analgesia
NAME OF PROCEDURE: Closed Reduction and Splinting of the *** metacarpal/s
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain and stiffness. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed with the procedure. A timeout was performed.
After IV analgesia was administered to the patient and provided adequate time for analgesic effect, the metacarpals were reduced using the Jahss maneuver under fluoroscopic guidance.
A well-padded ulnar/radial gutter/thumb spica gutter splint was then applied to the injured hand with care to maintain the hand in the intrinsic plus position. Fluoroscopic c-arm images showed improved alignment. The patient's neurovascular status was consistent with baseline.
NUMBER OF REDUCTION ATTEMPTS: ***
COMPLICATIONS: ***
DISPOSITION:
Discharged home with follow up with orthopaedic surgery in 1 week for repeat evaluation
PRE-PROCEDURE DIAGNOSIS: fracture of the *** metacarpal/s neck
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: IV analgesia
NAME OF PROCEDURE: Closed Reduction and Splinting of the *** metacarpal/s
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain and stiffness. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed with the procedure. A timeout was performed.
After IV analgesia was administered to the patient and provided adequate time for analgesic effect, the metacarpals were reduced using the Jahss maneuver under fluoroscopic guidance.
A well-padded ulnar/radial gutter/thumb spica gutter splint was then applied to the injured hand with care to maintain the hand in the intrinsic plus position. Fluoroscopic c-arm images showed improved alignment. The patient's neurovascular status was consistent with baseline.
NUMBER OF REDUCTION ATTEMPTS: ***
COMPLICATIONS: ***
DISPOSITION:
Discharged home with follow up with orthopaedic surgery in 1 week for repeat evaluation
| Common ICD-10 Codes | Brief Description |
|---|---|
| S62.20 | Fracture of the first metacarpal bone, closed |
| S62.21 | Fracture of the first metacarpal bone, open |
| S62.30 | Fracture of other metacarpal bone, closed |
| S62.31 | Fracture of other metacarpal bone, open |
| S62.40 | Multiple fracture of metacarpal bones, closed |
| S62.41 | Multiple fracture of metacarpal bones, open |